Is perimenopause worse than menopause?
Perimenopause is an often overlooked aspect of the end of a woman's menstrual cycle. Many women worry about the risk of breast cancer once their menstrual periods stop. Read on to find out more about Perimenopause/Menopause and how you can deal with it.
Menopause vs Perimenopause; An Overview:
Most of us would be familiar with the menopause, but perimenopause is probably a new concept to most of us. Your gynecologists would diagnose you with menopause when you have not had menstrual periods for 12 months or more, in the absence of a pregnancy. While menopause is the natural biological endpoint of a woman’s fertility cycle, perimenopause refers to the period of change from regular menstrual periods to menopause itself. So what is interesting about this is that technically, all the so called menopause symptoms that we’re all familiar with, such as hot flashes, vaginal dryness, night sweats, are all actually symptoms of perimenopause. They tend to last during the period of change to menopause itself, and disappear after it has been reached.


As far as the cause of perimenopause is concerned, it is pretty much the same as menopause itself. To better understand this, we must keep in mind the main parts of the female reproductive system. It consists of two ovaries and a uterus, which all make various hormones that control the menstrual cycle. Normally, during regular periods, the ovary produces two main hormones, called estrogen, and progesterone. The levels of these hormones in our body, is what controls the menstrual cycle, and also what indirectly controls the production of other hormones too, like thyroid hormones, and even insulin. They even affect calcium levels in our blood, as well as cholesterol levels.
Menopause Symptoms Demystified:
Usually, with increasing age, the ovaries start to make and release lower quantities of estrogen and progesterone, the two main female reproductive hormones. This is what starts the process of menopausal transition or perimenopause. It is the quantities of these very same hormones that are directly or indirectly responsible for perimenopause or menopause symptoms as well. The complex mechanisms of the female body’s reproductive system are thrown into chaos by the reduced estrogen and progesterone levels.
This in turn leads to the vasomotor symptoms, the most well-known of which, are hot flashes and night sweats. It also results in some degree of emotional distress during the time of perimenopause, as well as weight gain and dyspareunia due to the vasomotor symptoms themselves. Dyspareunia, or pain during sexual intercourse, is a common symptom that many women going through perimenopause experience, and are distressed by. However there is not nearly enough attention or mainstream medical research in this avenue.
How to cope with the symptoms of perimenopause?


It is definitely a myth that only 50 year old women have to deal with perimenopause or menopausal symptoms. It has been estimated that 1 in 100 women can experience premature menopause, which is menopause that begins much earlier than most cases. Premature menopause can set in any time after thirty years. Yes, you read that right. This early menopause can be due to a number of reasons, such as genetic reasons or primary ovarian failure. But apart from genetics, the commonest causes are usually due to the side effects of necessary surgeries, such as a hysterectomy or the removal of the ovary. While women in these cases are often on hormone therapy, the varying levels of estrogen and progesterone in their bodies can lead to premature menopause setting in.
Both in the case of early menopause and regular perimenopause, the role of a healthcare provider cannot be overstated. Apart from being the one to diagnose menopause, they also have a key role to educate and advice women who are experiencing unexplained weight gain, irregular menstrual cycles, and hot flashes. In this scenario, a healthcare provider has a similar importance as screening for breast cancer in women. It can be a very daunting and shocking experience to have your body do things which to you are unpleasant and unexpected. It is shocking that not too many years ago, the discomfort experienced by women all over the world during perimenopause was considered to be routine, and not something that required medical attention. Thankfully, modern medicine has evolved to the point where we stop thinking in such terms. But what exactly can be done?
In case of surgery or primary ovary failure, as previously mentioned, hormone therapy has a major role to play in delaying perimenopause. But the downside is that hormone therapy has side effects. Hormone therapy is also expensive, and requires regular checkups and monitoring by a healthcare provider. So it obviously is not a feasible option for most women. However it is essential to take extra care during perimenopause, because during normal menstrual cycles, estrogen has a lot of beneficial effects. Estrogen is cardioprotective, and prevents both breast cancer and osteoporosis in younger women. This is why fewer women have heart attacks, and also why osteoporosis is normally only something that is a disease that affects older women.
Non-steroidal alternatives to hormone therapy:
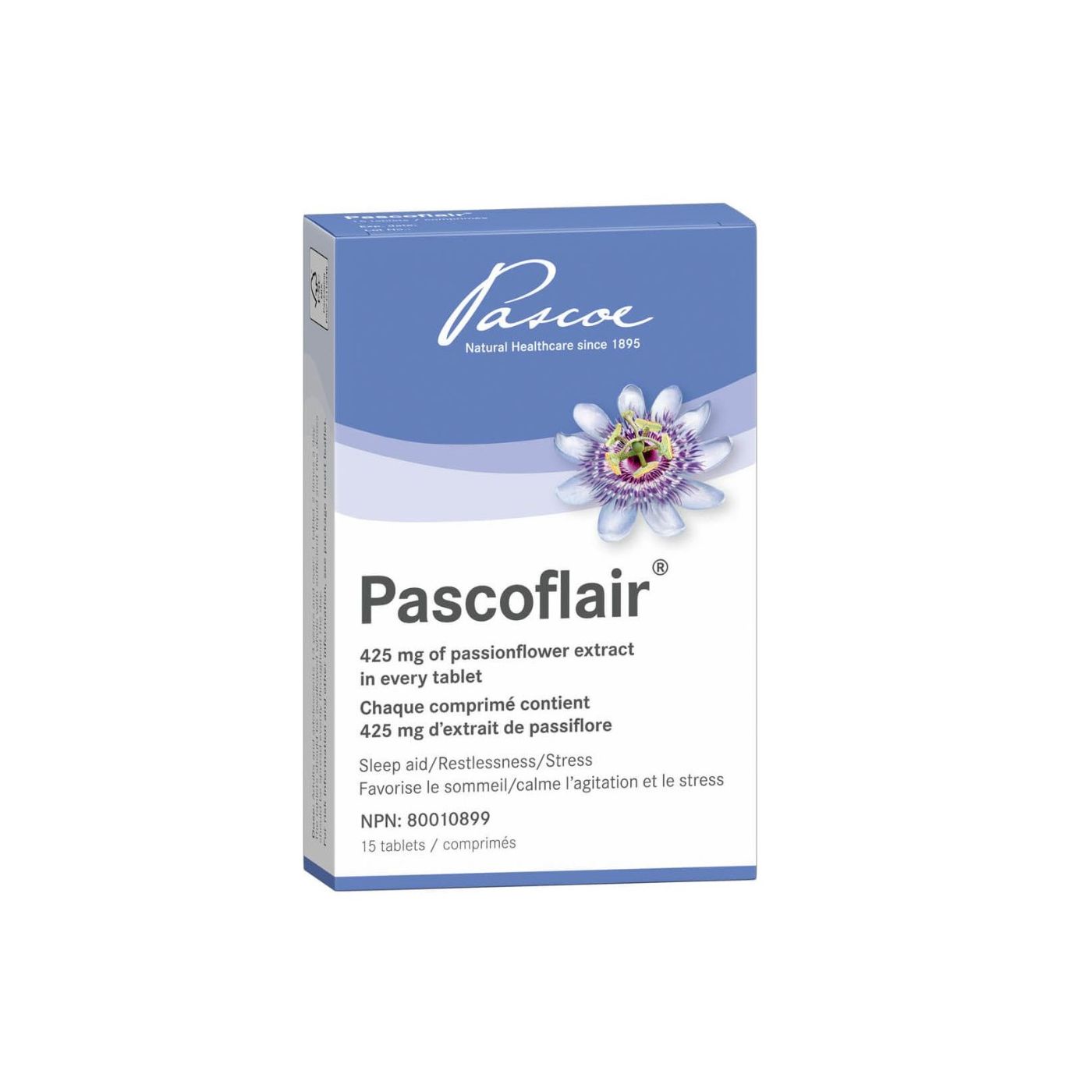
Since estrogen is itself a steroidal hormone, it is only natural that hormone therapy has side effects. Weight gain, hot flashes, emotional distress and other symptoms similar to menopausal symptoms are seen due to fluctuating estrogen levels. This is why hormone therapy is only a viable option for certain special situations. But these days, thankfully, there are many nonhormonal and non-steroidal options available. One does not have to simply endure hot flashes and keep worrying about heart attacks or breast cancer. There are plenty of herbal supplements that can help to alleviate menopausal symptoms, which have varying efficacy.
What works for one person, might not necessarily work for another person facing the same problems. It is through a process of trial and error that one ends up finding the right combination of supplements and medication that works the best. Since allopathic medicine is limited to pain killers and estrogen pills, these herbal alternatives range from Ayurvedic to homoeopathic medicines. The advantages of these are that they are also often GMO free and vegan friendly. Additionally, once you find out that there are so many avenues available to explore and benefit from apart from the remedies that are supplied by big pharmaceutical conglomerates, you end up finding solutions to other medical problems beyond allopathic medicine’s reach, too.


The Various Advantages of Nonhormonal Remedies:
Apart from the non-hormonal aspect of these options, Perhaps the best part of these alternative remedies, is that they have no side effects. The NAMS (North American Menopause Society) has recommended hypnosis for the treatment of perimenopause symptoms, for the very same reason. Even if they have varying efficacy, they pose no harm. And one of the fundamental principles of medicine is Primum non nocere which translates to: First, do no harm. This is why it is logical to give alternative or complementary medicine options a try. After all, they are basically low risk, high reward options. Particularly so, in any cases where the allopathic options available are not enough. There are far too many cases where the patients feel that the medication they are receiving isn’t sufficient to manage their symptoms. Such outliers often find relief in the avenues of alternative remedies.
Additionally in the era of COVID-19, it is also risky to visit hospitals and pharmacies. So it makes sense to avoid using techniques that are known to have harmful side effects, and try out complementary and alternative medicine. But as always, it is important to source such remedies from a reputable source, as there is no shortage of shysters on the internet who will try to sell you everything, from instant hair loss reversals to the cure for breast cancer.
Perimenopause Is Not A Disease:
With all the mention of risks of breast cancer and heart disease associated with decreased estrogen, one might assume that perimenopause is something to be frightened by. It is not. All that it is, is a biological process that every woman undergoes, at different ages, with different symptoms, at their own pace. Some menopausal women might experience intense hot flashes, and sleep issues. They might need to take Brisdelle or another drug to get some relief from their vasomotor symptoms.
Other menopausal women might have weaker weight bearing bones and thus be more likely to get osteoporosis and pathological fractures. Yet other women might, due to a combination of genetics and an altered hormonal state, be more susceptible to breast and endometrial cancer. They may even develop cancer of the ovary. But these are the worst case scenarios. And we must always keep in mind that worst case scenarios are more a function of probability than any one acquired factor.


Ultimately, perimenopause is an inevitable state of menopausal transition. Today, with a combination of allopathic and complementary medicine, it is better understood, and much easier to manage. Gone are the days when hot flashes, hot flushes, and vaginal dryness led to dyspareunia, discomfort and discord. These days it is much easier to approach your healthcare provider with such concerns, and they have finally been recognized as legitimate concerns.
And moreover, you now have the freedom to take your health into your own hands. Today, it is easy to learn more about menopause, and access alternative remedies from the comfort and safety of your own home. You can even have most of them delivered to your doorstep. This is a definite necessity in these trying times, due to the global COVID-19 pandemic. With increased education and awareness as well, perimenopause is no longer a cause for pause. Finally, perimenopausal women can undergo the twilight years of their menstrual cycle with comfort and dignity.